1. Breakdown of all the new CMS codes
2. Real billing examples
3. Sample 2-month proforma
4. Medicare billing requirements
5. Strategies to stack codes and bill navigation services monthly
Learn how to unlock over $100K in annual revenue per provider by billing for cancer patient navigation services using the new 2024 CMS codes
 LIVE
LIVE
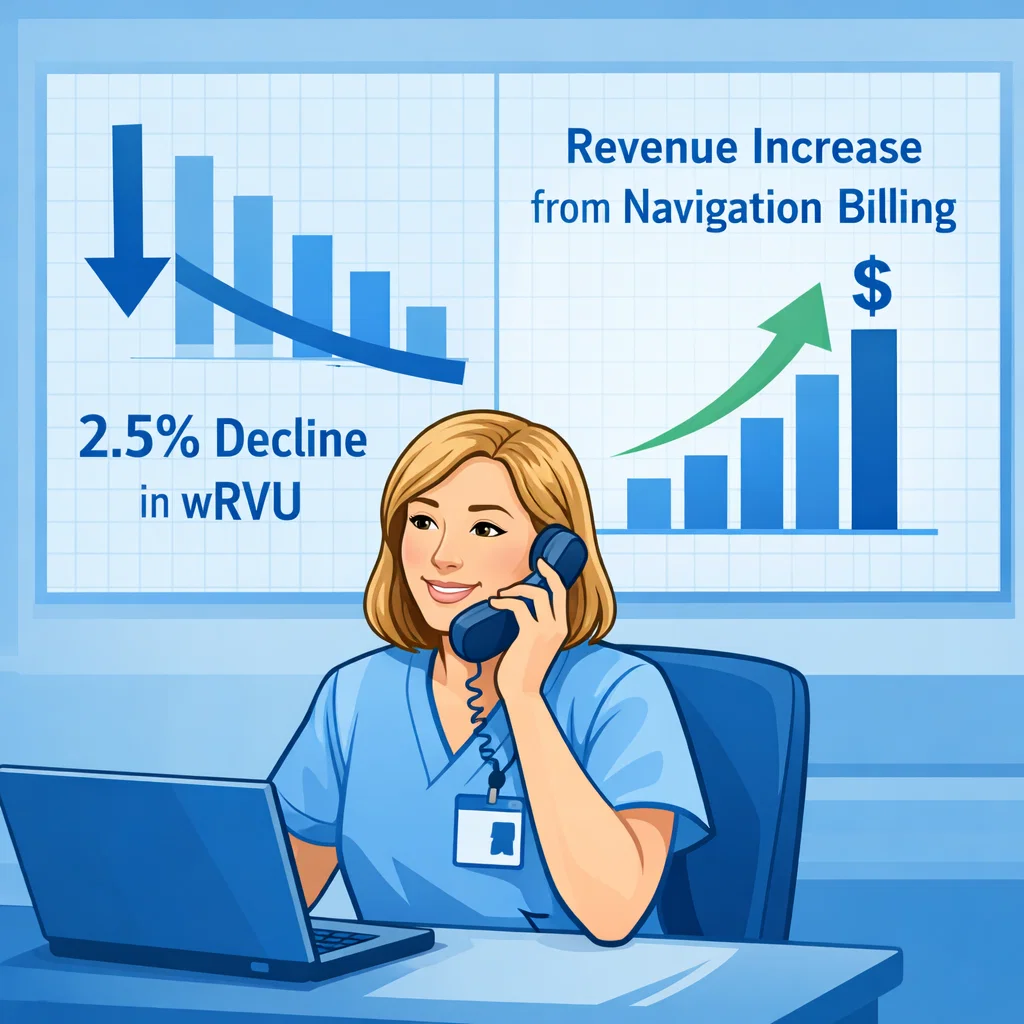
Oncology Practice Economics in 2026: From wRVU cuts to Sustainable Navigation Revenue
Register Now