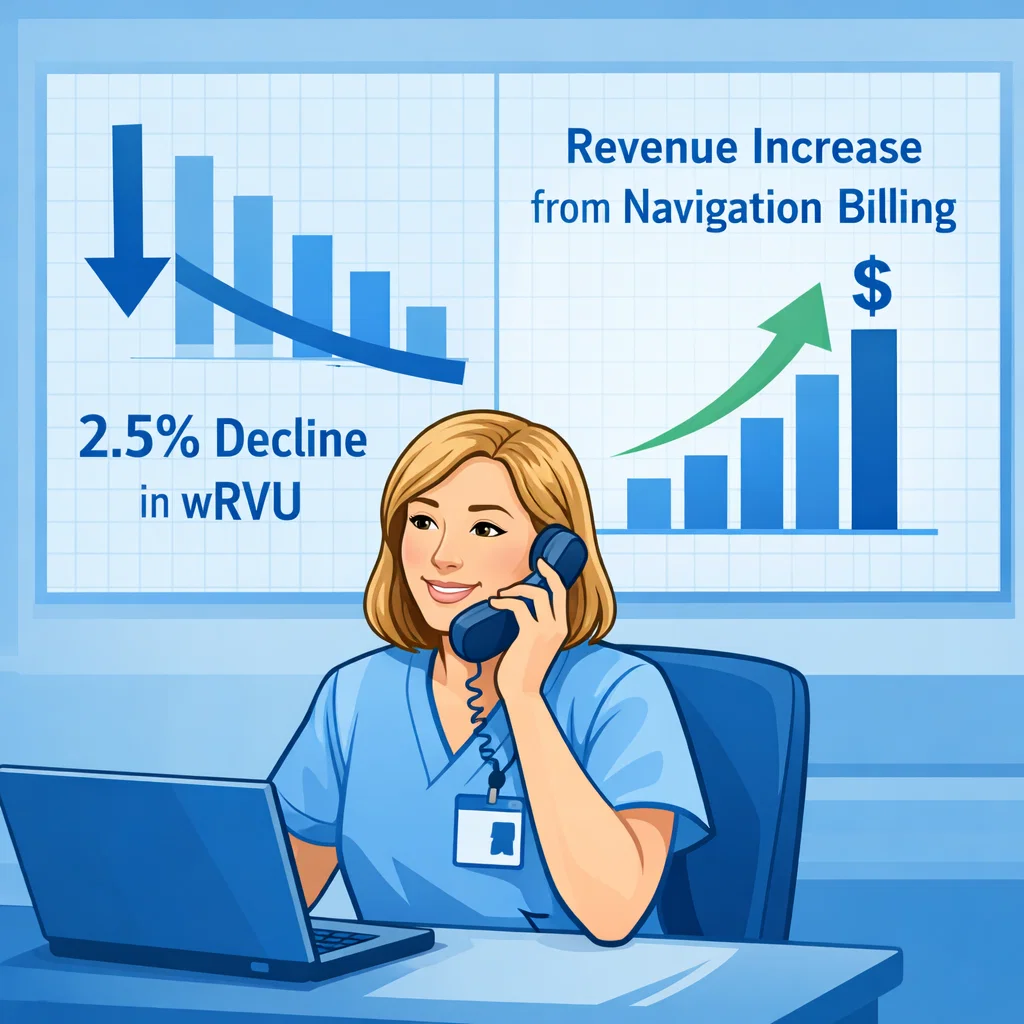
On January 1, 2026, Medicare reimbursement for cancer specialists will decline—even if your workload stays exactly the same.
This is because CMS has implemented a 2.5% cut to work RVUs, and has signaled its intention to repeat this reduction every three years going forward. For any oncology program where physician compensation, productivity, or contractual bonuses are tied to wRVUs, this is not a small adjustment—it is a direct pay cut on Day 1 of 2026.
Why is this happening?
CMS claims that physicians—surgeons in particular—are becoming more “efficient” and therefore require fewer RVUs for the same procedures. But real-world data tells a different story. The American College of Surgeons (ACS) has aggressively challenged this logic, submitting extensive comments and publishing a landmark study in the Journal of the American College of Surgeons showing that over 90% of operations are taking just as long or even longer than before. Despite clear evidence, CMS finalized the rule, moving ahead with across-the-board RVU reductions.
For oncology practices already dealing with shrinking margins, rising staffing costs, and increasingly complex patient populations, the impact of these cuts is unavoidable—and potentially destabilizing. Unless you take proactive steps now, your practice will enter 2026 with lower revenue, lower wRVU credit, lower compensation, and no reduction in clinical workload.
The Most Immediate Path to Replace Lost RVUs: Bill for Cancer Patient Navigation
While RVUs are dropping, CMS has simultaneously expanded reimbursement for patient navigation, care management, community health integration, and SDoH-related services—the very services oncology programs provide every day but rarely bill for.
If oncology practices want to stabilize revenue in 2026 and beyond, they must begin treating navigation as a billable clinical discipline, not a cost center.
That means:
- Hiring or formally designating a cancer patient navigator
- Building a repeatable workflow for assessments, education, coordination, SDoH review, follow-up, and treatment tracking
- Documenting every navigation encounter with timestamped activities (5–10+ billable touches per patient per month is typical)
- Using the navigator’s credentials strategically (RN vs. non-RN) to maximize eligible CPT codes
- Charging for every appropriate navigation service, just as you would for a medical visit or procedure
Oncology practices that operationalize navigation as a billable service routinely see $300–$600+ in new revenue per active cancer patient each month—often enough to fully fund a navigator’s salary within weeks.
And unlike the RVU cuts, navigation billing scales up, not down, over time.
Where XpediteMD Helps
XpediteMD provides oncology practices with the turnkey infrastructure needed to capture, track, and bill navigation encounters automatically. The platform includes:
- AI-powered ambient capture of navigation activities
- Role-based CPT code mapping
- Real-time encounter logging
- Navigation consent, risk, and SDoH workflows
- Automated billing documentation
- Full visibility into navigator productivity and revenue
Practices that adopt XpediteMD typically start generating navigation revenue within the first 30 days—precisely when RVU credits are falling.
Next Step: Learn What Top Cancer Practices Already Do
If you want to understand how leading oncology centers are getting ahead of the 2026 Medicare cuts, don’t miss our companion article:
4 Things Top Cancer Practices Do to Streamline and Maximize Navigation RevenueIt outlines the exact workflows, staffing models, and documentation behaviors that separate high-performing programs from everyone else.